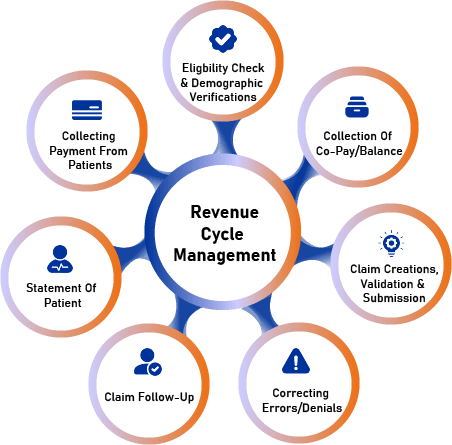
(RCM) is the process used by healthcare systems to track revenue from patients from their initial appointment or encounter with the healthcare system to their payment of balance.

Provides easy online payment options and monitors direct deposits and outstanding balances instantly and automatically. Collects reimbursement from all available medical and dental benefits, confirms that appropriate codes are selected from current code sets, and ensures all supporting documents are attached for successful claims. Streamlines your revenue cycle management process, reducing administrative burdens and freeing up staff to focus on patient care. Identifies and corrects errors, reducing denials and rejections, and ensuring timely payment.
Offers customized reporting and analytics to help you make informed decisions about your practice. Provides expert guidance on coding, compliance, and regulatory issues. Helps you stay ahead of industry changes and updates, ensuring you’re always in compliance. Increases cash flow and reduces bad debt with our proactive approach to accounts receivable management. Saves you time and money by reducing paperwork, phone calls, and other administrative tasks.
Automates tasks such as claims submission, payment posting, and denial management, freeing up staff to focus on higher-value tasks. Streamlines workflows and reduces manual errors, ensuring accuracy and efficiency. Improves productivity and reduces costs with automated processes.
Provides real-time visibility into revenue cycle performance, enabling data-driven decisions and process improvements. Offers customizable dashboards and reports to track key performance indicators. Enhances transparency and accountability with automated tracking and reporting.

Optimizes patient registration and scheduling processes to ensure accurate data capture and reduce errors.
Verifies patient eligibility and benefits in real-time, reducing denials and improving upfront collections.
Captures and resolves billing discrepancies at the point of service, minimizing rework and bad debt.
Improves patient engagement and satisfaction with clear communication of financial responsibilities and estimates.
Enhances staff productivity and efficiency with streamlined workflows and automated tasks, reducing bad debt and improving cash flow
Ensures accurate and complete coding and charge capture, reducing claim denials and improving revenue
Manages prior authorization and utilization review processes, ensuring compliance and reducing delays in care.
Provides patient financial services, including billing, payment processing, and financial counseling.
Streamlines claims management and denial prevention, reducing rework and improving revenue.
Utilizes data analytics and reporting to identify trends, monitor performance, and drive continuous improvement.


Providers generate claims to detail services rendered and associated codes (e.g., CPT and ICD-10).
Once providers have completed a claim, they send it to payers for reimbursement.
To assess the effectiveness of the revenue cycle, providers can track KPIs such as:
Back-end revenue cycle helps providers close the loop when it comes to patient accounting. To optimize the back-end revenue cycle, providers should:
Artificial Intelligence, Machine Learning, Robotics, and Cloud Computing transform industries with innovative solutions and efficiency.
Comprehensive evaluation of physical, emotional, and psychological well-being for personalized healthcare and wellness strategies.
Ongoing evaluation and refinement of processes, products, and services to enhance quality and efficiency.
Interdisciplinary teamwork and open communication to achieve shared goals and drive business success.
The Revenue Cycle Management process involves managing the administrative and clinical functions of a healthcare organization to ensure efficient and effective revenue generation. The process typically includes the following stages:
Don’t miss our future updates! Get Subscribed Today!
© Claim Bills 2025. All Rights Reserved.