Accelerate Your Cash Flow with Adean RCM Services
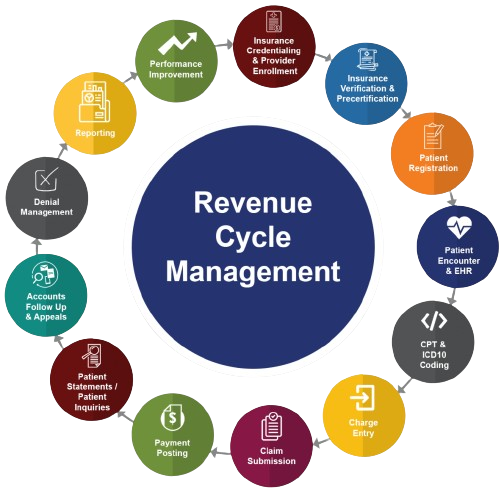
At Adean Medical Billing, we understand that maintaining a healthy cash flow is crucial for the success of your healthcare practice. Our Revenue Cycle Management (RCM) Services are specifically designed to accelerate your cash flow by optimizing every step of the revenue cycle. From patient registration to final payment posting, we employ advanced technologies and proven methodologies to ensure timely and accurate billing. Partner with Adean RCM Services to streamline your revenue cycle and focus on what you do best—providing exceptional patient care.