Revenue Cycle Management in USA 2025 will see big changes. New technologies, patient needs, and rules will shape how healthcare handles money.
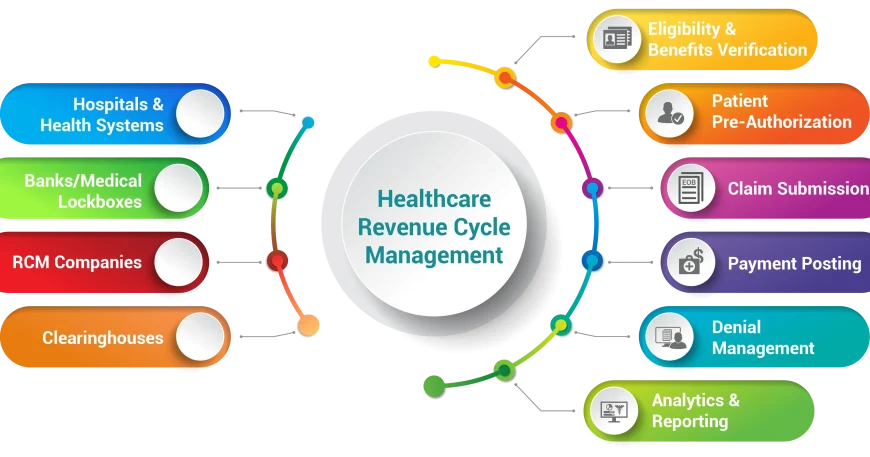
RCM systems have long helped with billing and managing claims. But, AI, ML, and digital tools are changing RCM. These technologies will make tasks easier, improve claims, and make finances easier for patients.

The COVID-19 pandemic has made RCM even more important. Healthcare groups that follow new RCM trends will stay financially strong. They will also make patients happier and follow new rules better.
Key Takeaways
- Artificial intelligence and machine learning will transform RCM through automation, predictive analytics, and real-time eligibility verification.
- Digital patient engagement tools, such as self-service payment platforms and mobile-first solutions, will enhance the patient financial experience.
- Regulatory compliance and security measures will be critical in safeguarding sensitive healthcare data and ensuring adherence to industry standards.
- Workflow optimization and end-to-end process automation will streamline RCM operations, leading to increased efficiency and cost savings.
- The future of RCM in the USA will be defined by a seamless integration of technology, regulatory updates, and patient-centric strategies.
The Evolution of Healthcare Revenue Cycle Management
The healthcare industry has seen big changes in its revenue cycle management (RCM) systems. It used to rely on manual processes and paper records. Now, it’s all about digital solutions and making decisions based on data.
Historical Development of Revenue Cycle Management Systems
Before, healthcare providers faced slow and error-prone RCM processes. Tasks like patient registration and claims submission were done by hand. This led to mistakes, delays, and less money coming in. But, the arrival of electronic medical records (EMRs) and billing software changed everything. It made RCM faster and more accurate, helping healthcare finances improve.
Current State of Revenue Cycle Management
Now, revenue cycle management in healthcare is much more advanced. It uses new technologies to make things more efficient and accurate. Things like electronic claims, automated checks, and data analysis have changed how finances are managed. This digital shift has helped providers cut costs, improve their finances, and make patients happier.
Key Drivers of Change in Healthcare Finance
- Shift towards value-based care and alternative payment models
- Increasing patient financial responsibility and the need for enhanced financial engagement
- Growing regulatory requirements and the need for robust compliance measures
- Advancements in artificial intelligence and machine learning capabilities
- Rising demand for seamless digital patient experiences and self-service payment options
The healthcare industry is always changing, and so is revenue cycle management in healthcare. These key drivers will shape the future. They will push providers to keep improving their financial strategies to stay ahead and stay financially strong.
| Historical RCM | Current RCM |
|---|---|
| Manual, paper-based processes | Automated, digital solutions |
| Inefficient, error-prone workflows | Streamlined, data-driven operations |
| Limited visibility and control over finances | Real-time analytics and enhanced financial management |
| Increased administrative costs and reduced revenue | Optimized costs and improved financial performance |
“The future of revenue cycle management in healthcare is about leveraging technology to drive efficiency, improve financial performance, and enhance the patient experience.”
Artificial Intelligence and Machine Learning Transforming RCM
The world of revenue cycle management (RCM) is changing fast. This is thanks to artificial intelligence (AI) and machine learning (ML). These new tools are set to change RCM in big ways, shaping what what’s revenue cycle management going to look like in 2025.
AI and ML are making a big difference in predictive analytics. They look at past data to predict and prevent claim denials. Predictive models can spot problems early, helping organizations act fast and make the claims process smoother.
AI is also making coding and billing easier. It helps reduce work for staff and makes sure everything is accurate. what’s revenue cycle management going to look like in 2025 will see even better tools for medical coding, leading to faster and more accurate payments.
AI and ML are also changing how RCM works. They help manage tasks better, making things more efficient and productive. They can catch problems quickly and help fix them fast, making RCM better.
Looking ahead to 2025, AI and ML will keep changing healthcare’s money side. They promise to make things more efficient, accurate, and proactive. This could take RCM to new levels of success.
“By 2025, AI and machine learning will be widely adopted in RCM, optimizing workflows, enhancing predictive capabilities, and automating administrative tasks to drive greater financial performance for healthcare organizations.”

Digital Patient Experience and Payment Solutions
The world of revenue cycle management is changing fast. Digital changes in how patients interact and pay for care are key for 2025. Healthcare providers are now using new ways to make things easier for patients and to handle money matters better.
Self-Service Payment Platforms
Self-service payment platforms are changing how patients handle their healthcare costs. These easy-to-use sites let patients see their bills, set up payment plans, and make payments whenever they want. This makes patients happier and helps staff do less paperwork.
Mobile-First Payment Solutions
More people are using their phones, so healthcare is moving to mobile payments. Patients can now pay, check their accounts, and set up automatic payments from their phones. This makes paying for care easier and faster.
Patient Financial Engagement Tools
Healthcare is also using special tools to help patients understand their costs. These tools give patients advice, payment options, and learning resources. This helps patients deal with healthcare costs better and supports better revenue cycle management in 2025.
The future of healthcare will depend on digital solutions for patients and payments. By using these new technologies, healthcare providers can make patients happier, make things run smoother, and do better financially.

| Digital Patient Experience and Payment Solutions | Key Benefits |
|---|---|
| Self-Service Payment Platforms | Improved patient convenience and control Reduced administrative burden for healthcare staff Enhanced patient satisfaction and timely payments |
| Mobile-First Payment Solutions | Seamless integration with patient’s mobile devices Increased payment accessibility and convenience Improved patient engagement and financial management |
| Patient Financial Engagement Tools | Personalized financial guidance and support Enhanced patient financial literacy and understanding Strengthened patient-provider relationship |
“The integration of digital patient experience and payment solutions will be a key driver in shaping the future of revenue cycle management in 2025.”
Future of Revenue Cycle Management in USA 2025
The healthcare industry in the United States is changing fast. By 2025, Revenue Cycle Management (RCM) will see big changes. New technologies, different consumer wants, and new rules will all play a part in these changes.
Artificial intelligence (AI) and machine learning (ML) will become more common in RCM. These tools will help make claims processing faster and more accurate. They will also help with data analysis, making RCM more efficient.
Healthcare providers will use AI to find and fix payment issues. They will also improve coding and billing. This will help patients understand their financial situation better.
The digital patient experience will also grow in importance. Patients will want easy, mobile payment options. They will want tools that help them manage their healthcare costs.
This means healthcare organizations will need to focus on user-friendly platforms. These platforms will help patients take charge of their financial health.
- Increased adoption of artificial intelligence and machine learning in RCM
- Enhanced digital patient experience and payment solutions
- Automation and workflow optimization across the revenue cycle
- Regulatory compliance and security measures to protect sensitive financial data
As we look to 2025, healthcare providers and RCM experts must adapt. They will need to use technology and data to improve their operations. This will help them give patients a better financial experience.
By keeping up with these trends, healthcare organizations can thrive. They will be ready for the changes in the RCM world.
“The future of revenue cycle management in the United States is poised for a remarkable transformation, with technological advancements and shifting consumer preferences driving a significant shift in the industry by 2025.”
Automation and Workflow Optimization in Revenue Cycle
Healthcare organizations are turning to automation and workflow optimization. They aim to make their processes smoother and more efficient. These changes include end-to-end automation, predictive analytics, and real-time eligibility checks. They promise to change how healthcare providers manage their revenue by 2025.
End-to-End Process Automation
End-to-end process automation is a big trend. It uses advanced tech to automate parts of the revenue cycle. This includes everything from patient registration to claim submission. It cuts down on errors and lets staff focus on important tasks.
Predictive Analytics in Claims Management
Predictive analytics is also making waves. It uses data and machine learning to predict claim denials. This helps improve cash flow and reduces work for staff. It looks at past data to spot patterns and offer insights in real-time.
Real-Time Eligibility Verification
Real-time eligibility checks are key too. They automate the process of checking patient insurance. This makes workflows smoother, cuts down on denials, and improves patient experience. It gives providers the info they need to make better decisions.
The future of revenue cycle management is all about automation, predictive analytics, and real-time checks. By adopting these, healthcare organizations will see better finances, less work, and happier patients.
Regulatory Compliance and Security Measures
The healthcare revenue cycle management (RCM) world is changing fast. Keeping up with rules and protecting data is now key. The industry is getting ready for new healthcare laws and data privacy rules like HIPAA.
Healthcare providers and RCM services need to be careful with patient data. They must use the latest security tools. This includes strong encryption, multi-step login, and plans for data backup and recovery. These steps help keep patient data safe and show you care about privacy.
Also, using AI and ML in RCM brings new challenges. You need to focus on keeping data private and making sure AI is used right. This helps you stay on top of changing rules and protect patient data. By doing this, you can lead in the future of healthcare revenue cycle management.
FAQ
What are the key trends shaping the future of revenue cycle management (RCM) in the USA by 2025?
By 2025, RCM in the USA will see big changes. Artificial intelligence and machine learning will become more common. Digital patient experiences and new payment solutions will also grow. Plus, rules and security will keep evolving.
How is artificial intelligence and machine learning transforming RCM processes?
AI and machine learning are changing RCM a lot. They help predict claim denials and automate coding. They also manage workflows better. These changes will make RCM more efficient and accurate by 2025.
What digital patient experience and payment solutions are shaping the future of RCM?
New payment platforms and mobile solutions are changing RCM. Self-service and mobile payments are making it easier for patients. These changes will make RCM more efficient.
How is the regulatory landscape and data security impacting the future of RCM?
New rules and data privacy are forcing healthcare to be more secure. They must protect patient info better. This will greatly affect RCM by 2025.
What are the key drivers of change in healthcare finance and their impact on RCM?
Healthcare finance is changing a lot. Value-based care, consumerism, and population health are key drivers. These changes will shape RCM and require new strategies.
How is end-to-end process automation and workflow optimization impacting RCM?
Automation and predictive analytics are changing RCM. They improve claims management and eligibility checks. These changes will make RCM more efficient and accurate by 2025.