Prior authorization, also referred to as pre-authorization or pre-certification, is a crucial step in the medical billing process that ensures healthcare providers receive insurance approval before delivering specific treatments, services, or medications. This process is necessary to confirm that the prescribed care is medically necessary and meets the insurance company’s criteria. Without proper authorization, patients may face denials or delays, and healthcare providers may experience reduced reimbursements or financial loss.
Why Is Prior Authorization Necessary?
Insurance companies use prior authorization to control healthcare costs and avoid unnecessary treatments. By reviewing the medical necessity of certain high-cost treatments, procedures, and medications, they ensure that patients are receiving appropriate care. This process helps eliminate fraud and abuse in healthcare by confirming the medical necessity before services are provided. However, the process can be complex and time-consuming, requiring close communication between healthcare providers and insurance companies.
In this article, we’ll explore the details of prior authorization, its importance in medical billing, and how practices can improve their workflow to minimize denials and delays.
What Is Prior Authorization?
Prior authorization is the process by which healthcare providers seek approval from an insurance company before providing certain treatments, medications, or procedures to ensure that they will be covered. Without this approval, claims for payment may be denied, leading to higher out-of-pocket costs for patients or financial losses for providers.
This process typically applies to services or medications that are more costly or have alternatives that may be more cost-effective. Examples include specialized medications, surgeries, and certain diagnostic procedures. By requiring pre-authorization, insurance companies aim to manage healthcare costs and encourage the use of appropriate and efficient treatments.
Common Services Requiring Prior Authorization
- Expensive prescription medications: Many brand-name drugs that have generic alternatives require prior authorization.
- Specialized treatments and procedures: High-cost medical procedures, such as surgeries or diagnostic tests, often require pre-authorization.
- Durable medical equipment (DME): Items like wheelchairs, prosthetics, or hospital beds frequently need authorization.
- Advanced imaging procedures: Tests like MRIs, CT scans, and PET scans typically require approval from insurers.
- Non-standard treatments: Treatments used off-label or for non-FDA-approved purposes may require additional scrutiny.
The Prior Authorization Process
The prior authorization process involves multiple steps, often requiring coordination between the healthcare provider, the insurance company, and the patient. Each step is crucial in ensuring that the treatment or service will be approved and covered by the patient’s health insurance plan.
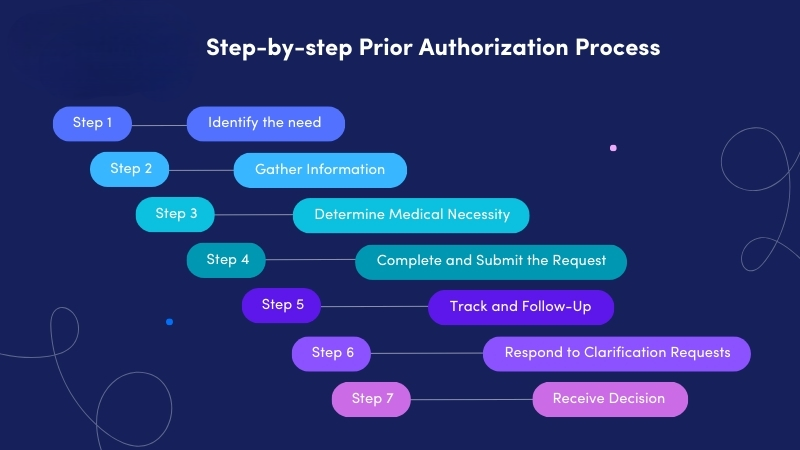
Step 1: Determining the Need for Prior Authorization
When a healthcare provider recommends a treatment or medication, the first step is verifying whether it requires prior authorization. This responsibility typically falls on the provider’s insurance verification or billing team, who must check the patient’s insurance eligibility and determine if the prescribed treatment falls under the insurance company’s prior authorization policy.
Step 2: Submitting the Request
Once it’s determined that prior authorization is required, the provider submits the necessary CPT (Current Procedural Terminology) codes and ICD-10 codes (used for the patient’s diagnosis) to the insurance company for review. These codes are essential as they provide specific information about the treatment or procedure that is being requested for coverage.
Step 3: Review by the Insurance Company
The insurance company’s review process may take several days to weeks, depending on the complexity of the request and the type of service. The insurance company evaluates whether the treatment is medically necessary and aligns with their guidelines. During this review, a panel of doctors, pharmacists, and healthcare professionals may assess the patient’s medical history and the potential cost-effectiveness of the proposed treatment.
Step 4: Approval or Denial
Once the insurance company completes its review, they will either approve or deny the request. If approved, the patient can proceed with the treatment, and the insurance company will cover the costs according to the terms of the patient’s plan. If denied, the healthcare provider and patient must decide whether to appeal the decision or explore alternative treatment options.
Step 5: Appeals Process
If a prior authorization request is denied, patients and providers have the right to appeal the decision. The appeals process requires submitting additional documentation to support the medical necessity of the treatment. It’s essential to provide thorough evidence, such as medical records and physician notes, to overturn the denial.
How Long Does Prior Authorization Take?
The length of time for the prior authorization process varies depending on the complexity of the request. While some approvals may come within 2-3 business days, others can take up to 10 business days or more. For urgent requests, insurance companies may expedite the review process, sometimes providing decisions within 24-48 hours.
Challenges of Prior Authorization in Medical Billing
Although prior authorization helps control healthcare costs, it often presents significant challenges for healthcare providers, patients, and billing teams. These challenges can lead to delays in care, administrative burdens, and potential financial losses.
1. Delays in Treatment
One of the most common criticisms of the prior authorization process is the potential for delays in treatment. Patients who require immediate care may face weeks of waiting before receiving the approval needed for coverage. This can worsen medical conditions and result in additional complications.
For example, some patients may be discharged from the hospital only to have their prescribed medication denied by their insurance. This can lead to rehospitalizations and further complications, as seen in real-life case studies.
2. Administrative Burdens
Healthcare providers and their billing teams must manage a significant administrative workload to comply with prior authorization requirements. The process often involves completing time-consuming forms, managing frequent follow-ups, and handling resubmissions for denied claims. This diverts resources away from patient care and increases the risk of human errors, which could result in claim denials or delays.
3. Risk of Denials
Even with the proper documentation and adherence to the process, denials may still occur. Some of the reasons for prior authorization denials include:
- Incorrect or missing information
- Disagreement on the medical necessity of the treatment
- Coding errors, such as incorrect CPT or ICD-10 codes
- Lack of documentation supporting the diagnosis
When denials occur, the appeals process can add further delays, and in some cases, the provider may need to absorb the cost of treatment if the claim is ultimately rejected.
The Impact of Prior Authorization on Revenue Cycle Management
In medical billing, effective revenue cycle management (RCM) is essential for maintaining a healthcare organization’s financial health. Prior authorization plays a critical role in ensuring that claims are processed and paid promptly, but mismanagement of the process can result in significant financial strain.
Reducing Denials and Rejections
One of the primary ways healthcare organizations can improve their RCM is by implementing systems that streamline the prior authorization process. By ensuring that pre-authorization requirements are met before services are rendered, healthcare providers can reduce denials, minimize delays in payment, and avoid the need for appeals.
Implementing Pre-Authorization Tools
Many healthcare providers are turning to practice management systems that integrate prior authorization tools. These tools can automate many aspects of the process, such as verifying insurance eligibility, checking for pre-authorization requirements, and submitting requests electronically. By automating these tasks, healthcare providers can reduce administrative burdens, improve accuracy, and speed up the authorization process.
Best Practices for Prior Authorization in Medical Billing
Managing prior authorization efficiently is key to reducing delays, improving patient care, and ensuring the financial health of healthcare practices. Here are some best practices for optimizing the prior authorization process:
1. Integrate Prior Authorization with Pre-Registration
Ensure that prior authorization is checked during the pre-registration phase of the patient’s visit. This will allow time for approvals and minimize delays when the patient is ready to receive treatment.
2. Utilize Electronic Health Record (EHR) Systems
Integrating prior authorization tools with EHR systems can streamline the process by automatically identifying when prior authorization is needed and submitting the required information to insurance companies. This reduces manual work and human errors.
3. Regularly Follow Up on Requests
Keep track of all pending prior authorization requests and follow up with the insurance companies regularly. This ensures that the process doesn’t stall and that approvals are obtained in a timely manner.
4. Provide Comprehensive Documentation
Ensure that all medical documentation is complete and accurate when submitting a prior authorization request. This reduces the chances of denials due to missing or incorrect information.
5. Train Staff on Prior Authorization Procedures
Provide ongoing training for staff responsible for handling prior authorization. Make sure they are familiar with the latest regulations, coding practices, and submission processes to avoid errors and delays.
Conclusion: Streamlining Prior Authorization for Better Outcomes
Prior authorization is a critical part of medical billing, ensuring that treatments and procedures are covered by insurance. While the process can be complex and time-consuming, it’s essential for preventing denials and ensuring appropriate care. By adopting best practices and integrating automated systems into their workflow, healthcare providers can streamline the prior authorization process, reduce delays, and improve both patient care and revenue cycle outcomes.
By staying informed and proactive, healthcare providers can navigate the challenges of prior authorization and ensure that they’re prepared to meet insurance requirements while minimizing disruptions to patient care.