Introduction
In healthcare, financial accuracy and regulatory compliance are critical. Medical billing audit services help healthcare providers identify and correct billing inaccuracies, reduce claim denials, and avoid costly penalties. Whether you’re a provider seeking to optimize your billing process or a healthcare administrator, understanding medical billing audit services is essential to ensuring compliance and maximizing revenue. Let’s dive into what medical billing auditing involves, why it matters, and how to choose the best options available.
What Is Medical Bill Auditing?
Medical bill auditing involves a systematic review of billing records to verify accuracy, compliance with healthcare regulations, and adherence to payer guidelines. Audits assess if billing codes are accurate, if medical services were documented correctly, and if payments align with services rendered. Regular audits prevent costly errors, reduce fraud risk, and ensure providers are fully reimbursed for their services.
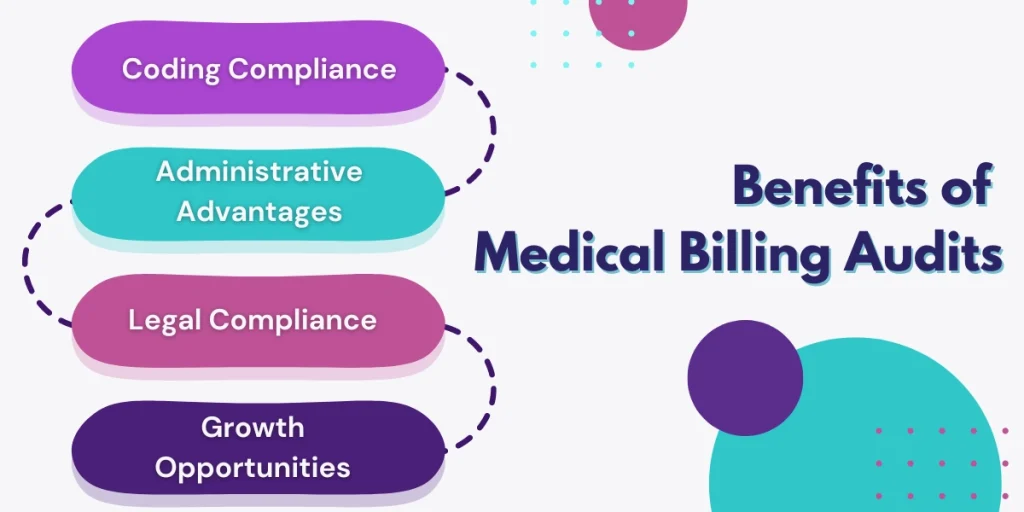
Key Benefits of Medical Billing Audit Services
- Enhanced Accuracy and Compliance: Regular audits help healthcare providers stay compliant with regulations, avoiding fines or penalties. An accurate billing process also builds trust with patients and insurers.
- Maximized Revenue: Identifying and correcting billing errors or inefficiencies can improve reimbursement rates, thus increasing revenue.
- Improved Operational Efficiency: Through audit insights, practices can streamline billing processes and improve accuracy, reducing time and labor costs associated with claim rejections.
- Reduced Fraud Risk: Medical billing audits help prevent fraudulent billing practices, safeguarding providers from legal issues and financial loss.
The Medical Billing Audit Process
The medical billing audit process is thorough and designed to evaluate every aspect of billing and claims management. Here’s a typical breakdown of the process:
- Initial Assessment: The audit begins with an assessment to identify goals, key areas of focus, and any past issues.
- Data Collection: Billing records, patient files, and coding documentation are gathered for review.
- Analysis: Auditors analyze the data, cross-referencing codes, services rendered, and payer guidelines to detect inconsistencies.
- Reporting: After the audit, the team provides a comprehensive report detailing findings, errors, and recommended actions.
- Implementation of Corrections: The findings help to correct any issues and improve future billing accuracy.
- Follow-Up Audits: Ongoing audits ensure that the implemented changes are effective and that compliance is maintained.
How to Do a Medical Billing Audit
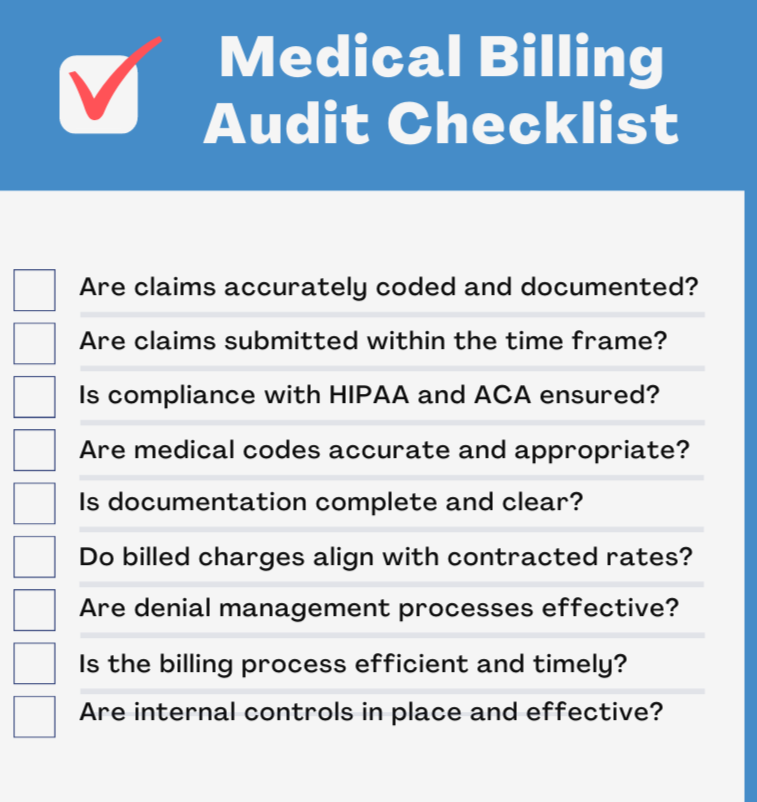
Performing a medical billing audit requires a systematic approach and an understanding of billing codes and regulations. Here’s a simple medical billing audit checklist to guide the process:
- Verify patient information and demographics.
- Check that all services billed are documented correctly.
- Ensure that CPT, ICD-10, and HCPCS codes are accurately applied.
- Confirm compliance with payer policies and regulations.
- Review claim denial and appeal processes to ensure accuracy.
For a more comprehensive medical billing audit, consider hiring medical billing audit experts or consulting a specialized medical billing audit consultant.
Types of Medical Billing Audit Services
- Insurance Medical Billing Auditing Companies: These specialize in auditing billing records specifically related to insurance claims, ensuring all documentation aligns with payer requirements.
- Medicaid Billing Audit: Medicaid billing audits ensure compliance with government guidelines, which is essential to avoid Medicaid fraud and ensure correct reimbursements.
- Comprehensive Medical Billing Audit: This involves a full audit of the provider’s entire billing system, from documentation to final claims submission, to assess accuracy, compliance, and efficiency.
- Specialized Services in Specific Locations: Some audit companies, like those offering medical billing audit services in Florida, provide regional expertise that can be beneficial for providers in that area.
Finding the Best Medical Billing Audit Services in USA
When searching for medical billing auditing companies or specific providers like medical billing audit companies in Florida, it’s essential to consider the following factors:
- Experience and Expertise: Look for companies with proven experience in healthcare auditing. The best medical billing audit companies have a team of certified auditors and medical coders familiar with the latest regulations and payer policies.
- Customization: Choose a provider that can tailor their services to meet the unique needs of your practice or specialty.
- Technology and Resources: The best audit companies leverage modern technology, such as automated software, to enhance accuracy and efficiency.
- Reputation and Reviews: Reviewing past client feedback and online medical billing audit services reviews can provide insight into the company’s reliability and effectiveness.
- Consulting Services: Some companies offer medical billing audit consulting to help you set up an internal audit program and train your staff, providing long-term benefits.
How to Audit Your Medical Billing Company
If you already work with an external billing company, it’s wise to conduct regular audits to ensure accuracy and compliance. Here are some tips for how to audit your medical billing company:
- Review Billing and Coding Accuracy: Ensure codes used match services provided.
- Analyze Reimbursement Rates: Confirm that reimbursements align with payer contracts.
- Monitor Denials and Appeals: Frequent claim denials may signal a need for process improvements.
- Evaluate Compliance with HIPAA and Payer Regulations: Verify that the billing company complies with all relevant regulations.
The Importance of a Medical Billing Audit Checklist
A medical billing audit checklist helps streamline the audit process, ensuring all necessary steps are followed. It allows for a structured approach that covers patient information, documentation accuracy, and billing code compliance, reducing the risk of errors.
Choosing Medical Billing Audit Experts for Peace of Mind
Hiring medical billing audit experts provides peace of mind, knowing that your practice’s billing is handled by professionals with a thorough understanding of regulations and industry standards. Professional auditors have the experience to quickly identify discrepancies and provide actionable recommendations.
Conclusion: Why Invest in Medical Billing Audit Services?
In today’s complex healthcare environment, accuracy, and compliance are essential for long-term success. Investing in regular medical billing audits allows healthcare providers to stay compliant, maximize reimbursements, and build trust with patients and insurers. By partnering with reputable medical billing audit services in the USA, healthcare practices can enjoy smoother operations, reduced financial risks, and more reliable revenue streams.



